Projects ECG (Electrocardiogram) Monitoring
Cardiomyopathy and Myocarditis
In the previous post Myocardial infarction, it was mentioned that Cardiomyopathy and Myocarditis have similar elements
to MI. Here I have summarized the main elements of Cardiomyopathy and Myocarditis.
Heart failure was also included as there were cases where heart failure was included in relation to the above
cardiopathy.
As with MI, there is no data on the pre-onset condition of the two diseases, so the analysis results are only for
reference.
There was a slight mistake regarding the s0423_re data introduced in the previous post on atrial fibrillation.
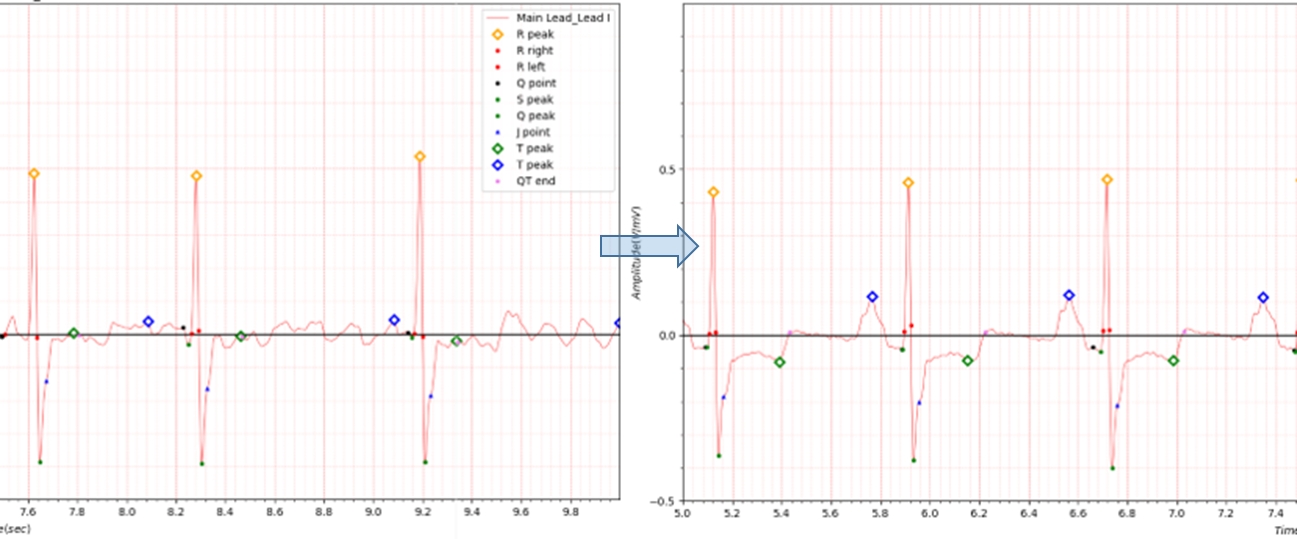
Fig.1 patient201 ECG date: 22/02/1996 -> 28/02/1996
patient201: s0420_re, s0423_re
- age: 39
- sex: male
- ECG date: 28/02/1996
- Reason for admission: Cardiomyopathy
- Acute infarction (localization): no
- Former infarction (localization): unknown
- Additional diagnoses: Atrial fibrillation, Hypertrophic cardiomyopathy
The ECG data in the PTB database has a head file like the one above. This is the result of misunderstanding the additional diagnostic term Atrial fibrillation.
1. Cardiomyopathy
What is cardiomyopathy?
Any disorder that affects the heart muscle is called cardiomyopathy. Cardiomyopathy causes the heart to lose its ability to pump blood well. In some cases, the heart rhythm also becomes disturbed. This leads to arrhythmias (irregular heartbeats). There are many causes of cardiomyopathy,
including:
- Alcohol abuse
- High blood pressure
- Coronary artery disease
- Viral infections
- Certain medicines
Often, the exact cause of the muscle disease is never found.
How does cardiomyopathy differ from other heart disorders?
Cardiomyopathy differs from many of the other disorders of the heart in several ways, including:
- Cardiomyopathy can occur in young people.
- The condition tends to be progressive. Sometimes it worsens fairly quickly.
- It may be associated with diseases involving other organs, as well as the heart.
- Dilated cardiomyopathy is a leading cause for a heart transplant.
- It is often the result of gradual changes of heart structure over time
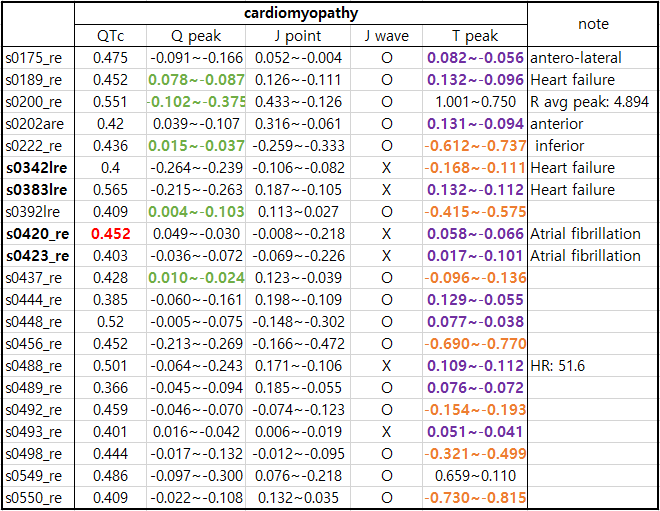
Table1. Cardiomyopathy
Note
Q peak: green color color Delta wave
T peak: purple color T wave positive and negative, orange color T wave reversed
patient127 s0342lre(ECG date: 26/10/1993), s0383lre(ECG date: 08/12/1993)
patient201: s0420_re, s0423_re
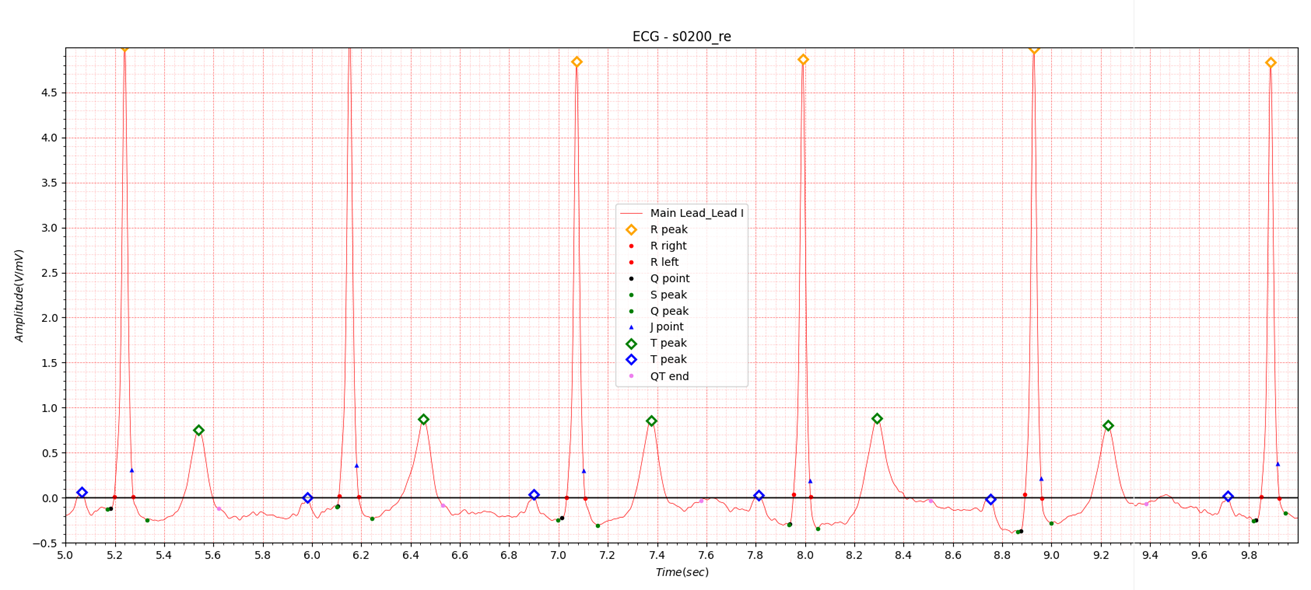
Fig.2 Hypertrophic obstructive cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle becomes thickened, also called hypertrophied.
The thickened heart muscle can make it harder for the heart to pump blood.
Many people with hypertrophic cardiomyopathy don't realize they have it. That's because they have few, if any, symptoms.
But in a small number of people with HCM, the thickened heart muscle can cause serious symptoms. These include shortness
of breath and chest pain. Some people with HCM have changes in the heart's electrical system. These changes can result
in life-threatening irregular heartbeats or sudden death.
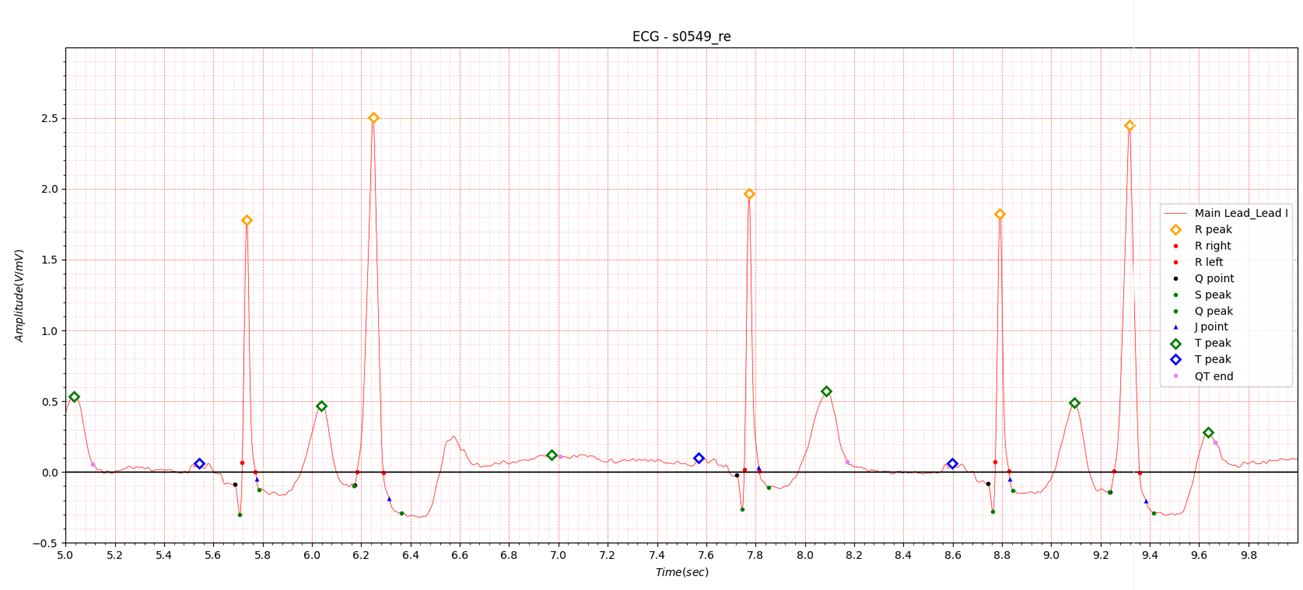
Fig.3 Dilated Cardiomyopathy(Recurrent ventricular tachycardias)
Symptoms
Some people with dilated cardiomyopathy don't have any signs or symptoms in the early stages of the disease.
Signs and symptoms of dilated cardiomyopathy may include:
- Fatigue
- Shortness of breath (dyspnea) during activity or while lying down
- Reduced ability to exercise
- Swelling (edema) in the legs, ankles, feet or belly (abdomen)
- Chest pain or discomfort
- Fast, fluttering or pounding heartbeat (palpitations)
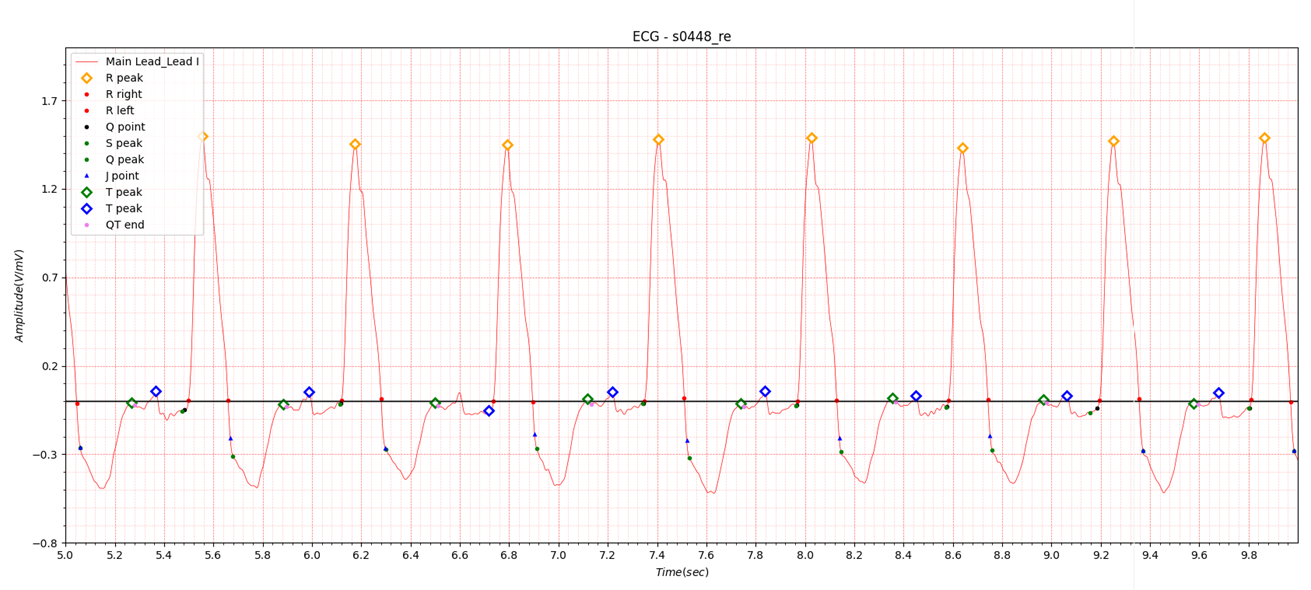
Fig.4 Dilated Cardiomyopathy
Complications
Complications of dilated cardiomyopathy include:
- Heart failure. The heart can't pump enough blood to meet the body's needs. Untreated, heart failure can be life-threatening.
- Leaky heart valves (heart valve regurgitation). Cardiomyopathy may make it harder for heart valves to close. Blood may leak backward through a heart valve.
- Irregular heartbeats (arrhythmias). Changes in the heart's size and shape can interfere with the heart's rhythm.
- Sudden cardiac arrest. Dilated cardiomyopathy can cause the heart to suddenly stop beating.
- Blood clots. Pooling of blood in the left lower heart chamber can lead to blood clots. If clots enter the bloodstream, they can block blood flow to other organs, including the heart and brain. Blood clots can cause stroke, heart attack or damage to other organs. Arrhythmias can also cause blood clots.
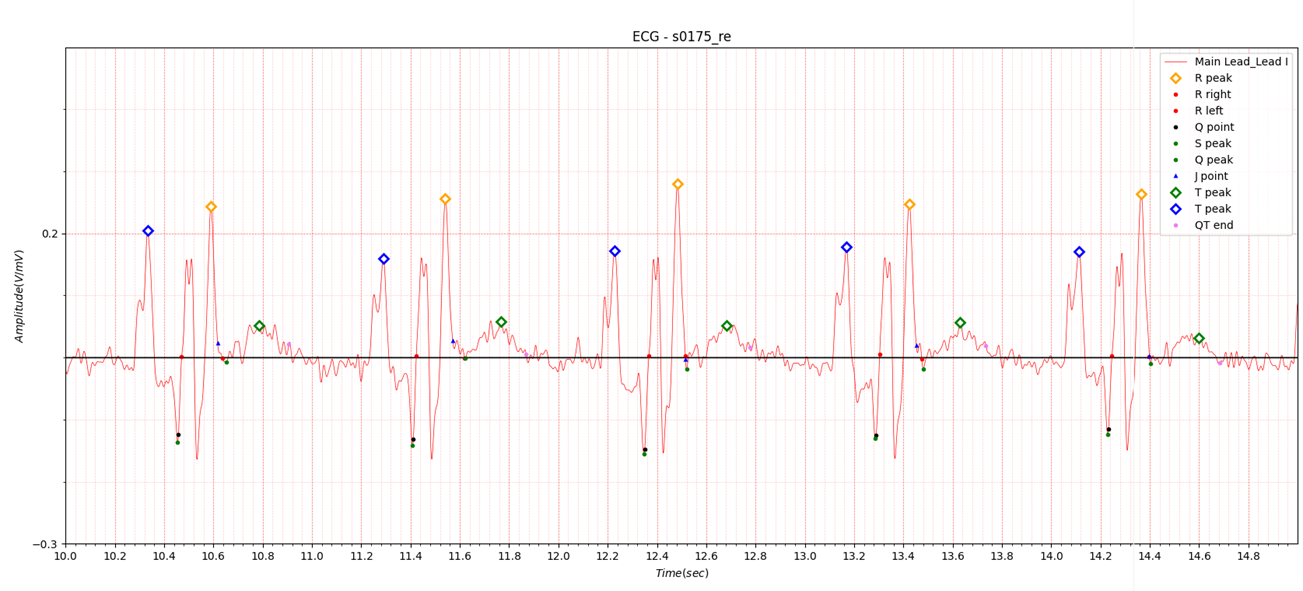
Fig. 5 s0175_re
S0175_re data has complex cardiopathy.
- Reason for admission: Myocardial infarction
- Acute infarction (localization): no
- Former infarction (localization): antero-lateral
- Additional diagnoses: Recurrent ventricular tachycardia, Dilated cardiomyopathy secondary to coronary artery disease, Hyperthyreosis
It is not easy to accurately detect the R wave peak position because there are three sharp peaks in a row.
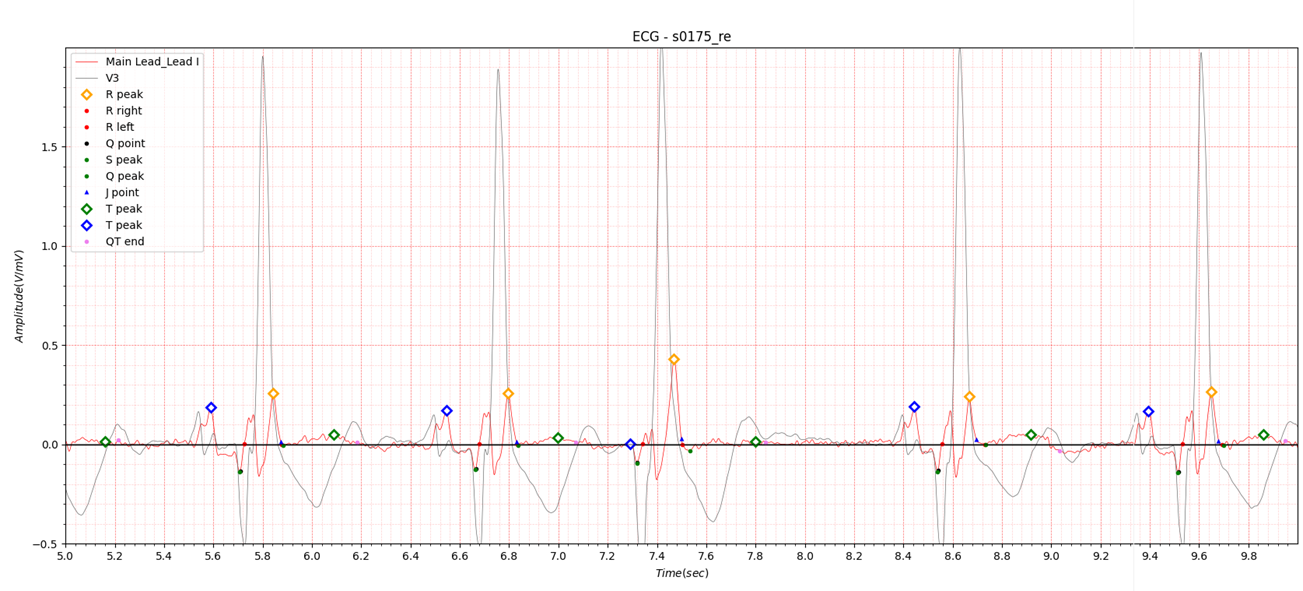
Fig.6 s0175_re Lead I and V3
In Fig.3 V3, the location of the R wave can be clearly seen.
You can see that the yellow diamond mark is R peak and the peak before that is R’.
Because other leads cannot be referenced in a single-lead ECG measurement system, finding the exact location of the R
peak is of utmost importance.
2. Myocarditis
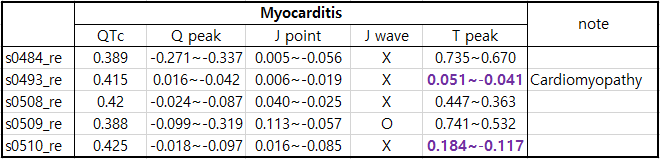
Table2. Myocarditis
Overview
Myocarditis is inflammation of the heart muscle, called the myocardium. The condition can reduce the heart's ability to
pump blood. Myocarditis can cause chest pain, shortness of breath, and rapid or irregular heartbeats.
Infection with a virus is one cause of myocarditis. Sometimes myocarditis is caused by a medicine reaction or a
condition that causes inflammation throughout the body.
Severe myocarditis weakens the heart so that the rest of the body doesn't get enough blood. Clots can form in the heart,
leading to a stroke or heart attack.
Treatment for myocarditis may include medicines, procedures or surgeries.
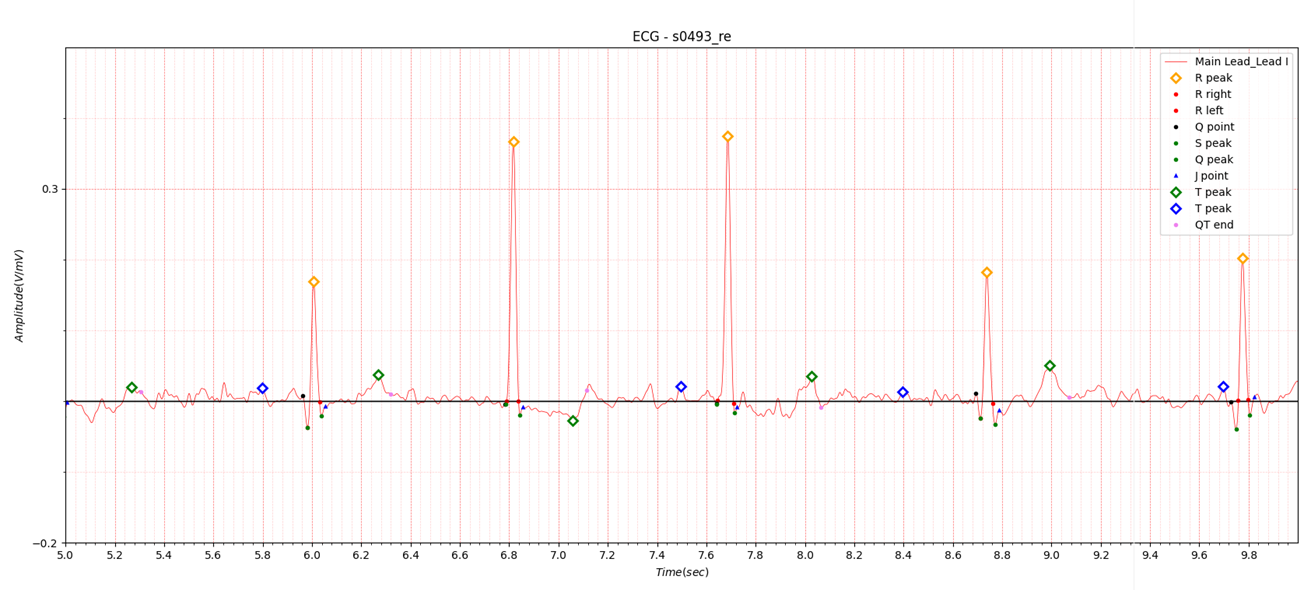
Fig.7 myocarditis
Symptoms
Some people with early myocarditis don't have symptoms. Others have mild symptoms.
Common myocarditis symptoms include:
- Chest pain.
- Fatigue.
- Swelling of the legs, ankles and feet.
- Rapid or irregular heartbeats, called arrhythmias.
- Shortness of breath, at rest or during activity.
- Lightheadedness or feeling like you might faint.
- Flu-like symptoms such as headache, body aches, joint pain, fever or sore throat.
3. Heart failure
Overview
Heart failure means that the heart is unable to pump blood around the body properly. It usually happens because the
heart has become too weak or stiff.
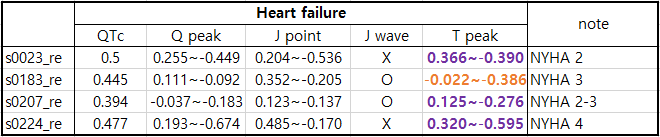
Table3. Heart Failure
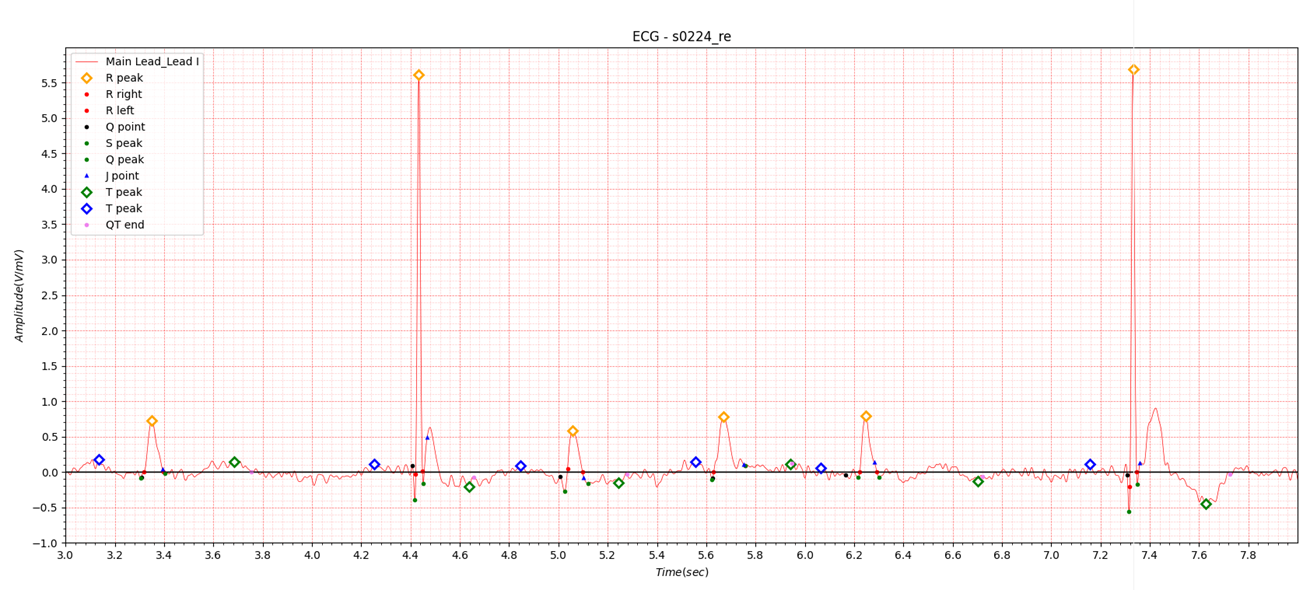
Fig.8 Heart Failure 1
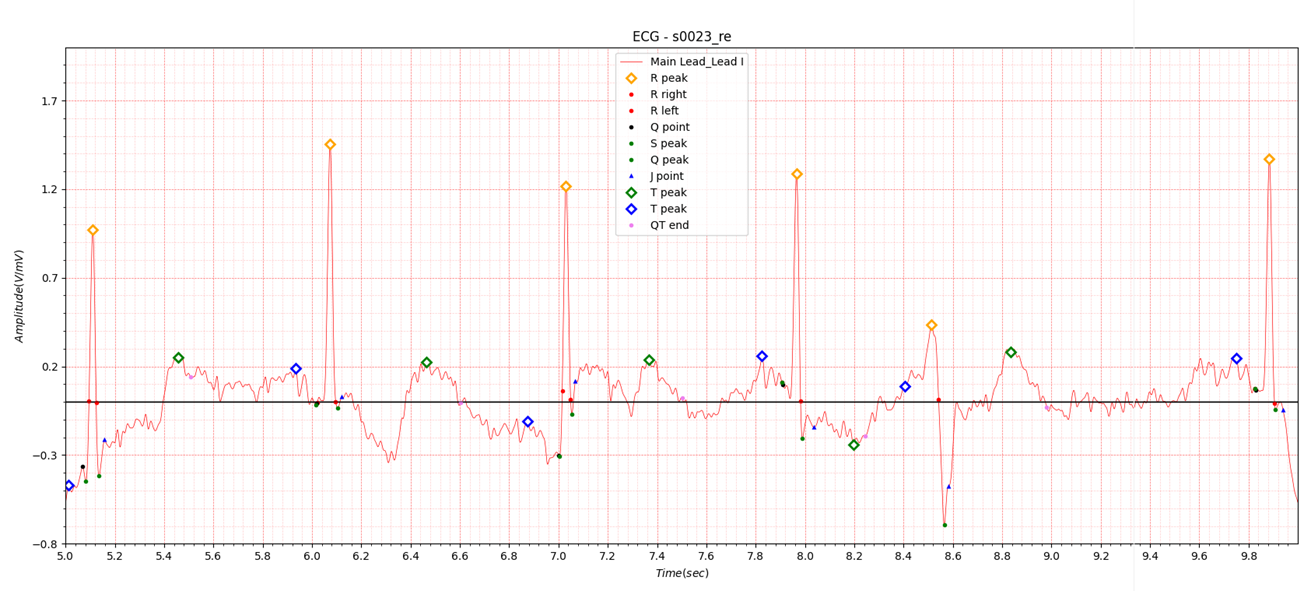
Fig.9 Heart Failure 2
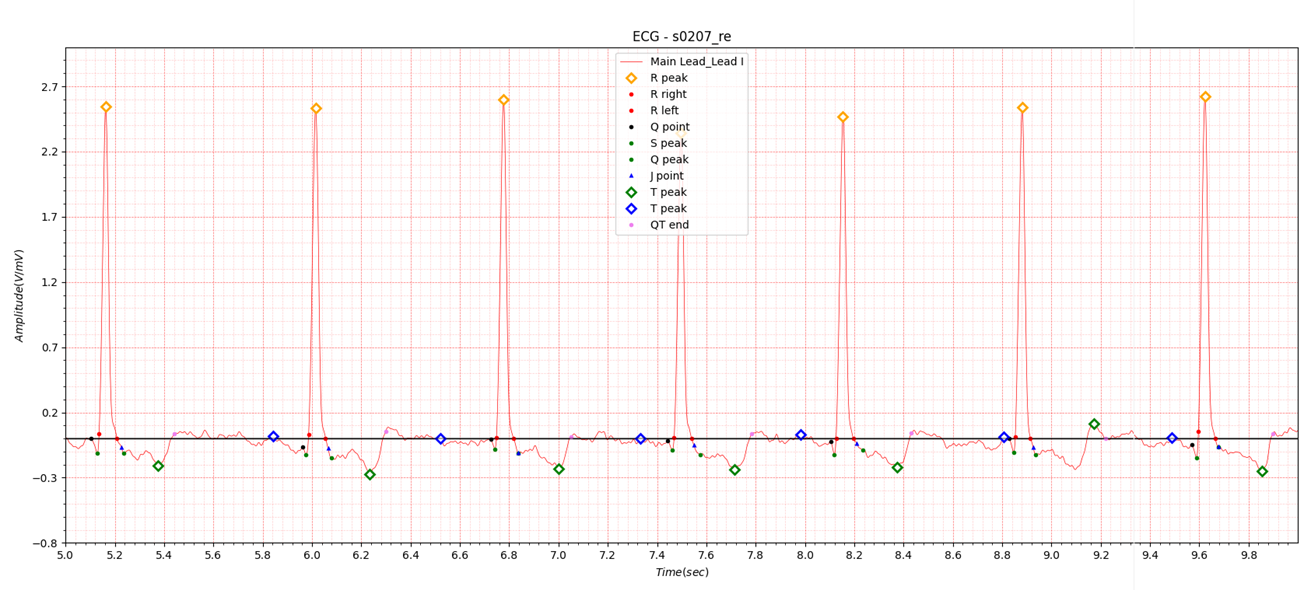
Fig.10 Heart Failure 3
References
1. cardiomyopathy
https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709
Types of cardiomyopathy include:
- Dilated cardiomyopathy. In this type of cardiomyopathy, the heart's chambers thin and stretch, growing larger. The
condition tends to start in the heart's main pumping chamber, called the left ventricle. As a result, the heart has
trouble pumping blood to the rest of the body.
This type can affect people of all ages. But it happens most often in people younger than 50 and is more likely to affect men. Conditions that can lead to a dilated heart include coronary artery disease and heart attack. But for some people, gene changes play a role in the disease. - Hypertrophic cardiomyopathy. In this type, the heart muscle becomes thickened. This makes it harder for the heart to
work. The condition mostly affects the muscle of the heart's main pumping chamber.
Hypertrophic cardiomyopathy can start at any age. But it tends to be worse if it happens during childhood. Most people with this type of cardiomyopathy have a family history of the disease. Some gene changes have been linked to hypertrophic cardiomyopathy. The condition doesn't happen due to a heart problem. - Restrictive cardiomyopathy. In this type, the heart muscle becomes stiff and less flexible. As a result, it can't expand and fill with blood between heartbeats. This least common type of cardiomyopathy can happen at any age. But it most often affects older people. Restrictive cardiomyopathy can occur for no known reason, also called an idiopathic cause. Or it can by caused by a disease elsewhere in the body that affects the heart, such as amyloidosis.
- Arrhythmogenic right ventricular cardiomyopathy (ARVC). This is a rare type of cardiomyopathy that tends to happen between the ages of 10 and 50. It mainly affects the muscle in the lower right heart chamber, called the right ventricle. The muscle is replaced by fat that can become scarred. This can lead to heart rhythm problems. Sometimes, the condition involves the left ventricle as well. ARVC often is caused by gene changes.
- Unclassified cardiomyopathy. Other types of cardiomyopathy fall into this group.
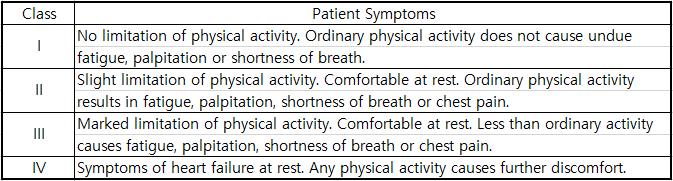
Classes and Stages of Heart Failure | American Heart Association
Stages of Heart Failure
In collaboration with the American College of Cardiology, the AHA has identified four stages of heart failure. They are described in the table below.
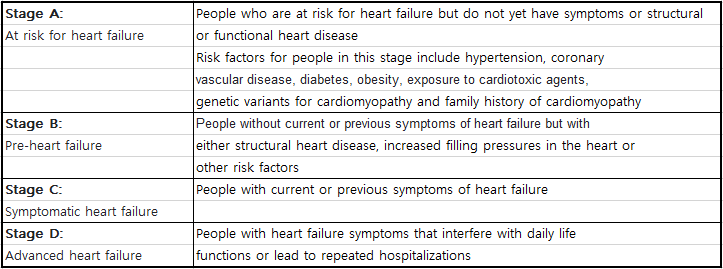
Classes of Heart Failure
By classifying patients in stage C and stage D heart failure, health care professionals better understand how to treat
people in these more advanced stages. Health care professionals typically classify patients' heart failure according to
the severity of their symptoms.
The most commonly used classification system, the New York Heart Association (NYHA) Functional Classification1, places
patients in one of four categories based on limitations of physical activity.
If you are diagnosed with stage C or stage D heart failure, your health care professional will give you an NYHA
Functional Classification as a baseline. Then, as you undergo treatment, your health care professional will assign
another classification of your condition, allowing your care team to measure how well treatment is working.
The table below describes the different classes in the NYHA Functional Classification.